For adults with moderately to severely active ulcerative colitis (UC) or Crohn’s disease (CD).
Support for your patients
We understand that each of your ENTYVIO patients may face unique situations while living with a chronic disease. EntyvioConnect offers a range of programs and services to support them throughout the insurance approval process once the prescribing decision is made.
Speak directly to a Case Manager at 1-855-ENTYVIO (1-855-368-9846),
Monday to Friday, from 8 am to 8 pm ET (except holidays).
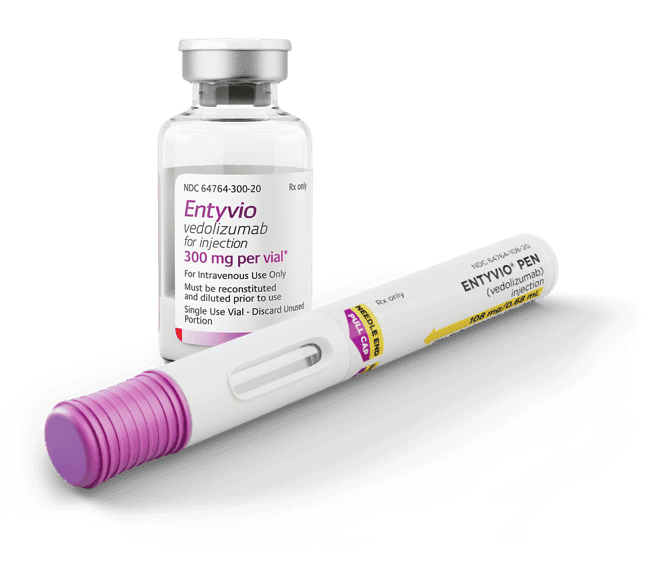
Over 90% unrestricted
commercial coverage for
ENTYVIO IV, and growing
coverage for the ENTYVIO Pen.*
Patients may remain on ENTYVIO IV until they
are covered for the ENTYVIO Pen. Discontinue
ENTYVIO in patients who do not show evidence
of therapeutic benefit by Week 14.1
The EntyvioConnect
Co-Pay Program may help
commercial patients pay as
little as $0 per dose† of
ENTYVIO up to the maximum
annual program benefit
IV=intravenous.
*For IV, unrestricted refers to coverage that does not require biologic step-edits. For pen, covered commercial lives include unrestricted coverage and biologic step-edits. Data are derived from Managed Markets Insight & Technology as of December 2024 (IV) and January 2025 (pen).
The EntyvioConnect Co-Pay Program ("Co-Pay Program") provides financial support for commercially insured patients who qualify for the Co-Pay Program. Participation in the Co-Pay Program and provision of financial support is subject to all Co-Pay Program terms and conditions, including but not limited to eligibility requirements, the maximum benefit per claim and the Maximum Annual Benefit. By enrolling in the Co-Pay Program, you agree that the program is intended solely for the benefit of you—not health plans and/or their partners. Further, you agree to comply with all applicable requirements of your health plan. The Co-Pay Program cannot be used if the patient is a beneficiary of, or any part of the prescription is covered by: 1) any federal, state, or government-funded healthcare program (Medicare, Medicare Advantage, Medicaid, TRICARE, etc.), including a state pharmaceutical assistance program (the Federal Employees Health Benefit (FEHB) Program is not a government-funded healthcare program for the purpose of this offer), 2) the Medicare Prescription Drug Program (Part D), or if the patient is currently in the coverage gap, or 3) insurance that is paying the entire cost of the prescription. Takeda reserves the right to change or end the Co-Pay Program at any time without notice, and other terms and conditions may apply.
If you have enrolled in an accumulator adjustment, co-pay maximizer, or similar program that purports to help manage costs or later learn that your insurance company or health plan has implemented such a program, you agree to inform EntyvioConnect at 1-844-368-9846. In an accumulator adjustment program, payments made by you that are subsidized by a manufacturer co-pay assistance program do not count toward your deductibles and other out-of-pocket cost-sharing obligations. In a co-pay maximizer program, the amount of your out-of-pocket cost obligation is increased to match support offered by a manufacturer co-pay assistance program. It may be possible that you are unaware whether you are subject to these programs when you enroll in the Co-Pay Program. Takeda will monitor program utilization data and reserves the right to discontinue assistance under the Co-Pay Program at any time if Takeda determines that you are subject to a co-pay maximizer, accumulator, or similar program.
The Maximum Annual Benefit under the Co-Pay Program is subject to change without notice. Subject to all terms and conditions, the Maximum Annual Benefit under the Co-Pay Program may be applied to out-of-pocket cost for your ENTYVIO prescription, including co-pay, co-insurance or deductible. The Co-Pay Program is for medication costs only and does not include costs to give you your treatment. Subject to all terms and conditions, the Maximum Annual Benefit under the Co-Pay Program is $20,000 per calendar year. However, except where prohibited by law, if your insurance company or health plan implements a co-pay maximizer program or similar program, you will have a reduced Maximum Annual Benefit of $9,000 per calendar year. If your insurance company or health plan removes ENTYVIO from such program, subject to all terms and conditions, you will be eligible for co-pay assistance up to the Maximum Annual Benefit for patients who are not subject to maximizer adjustment or similar programs.
The actual application and use of the benefit available under the co-pay assistance program may vary on a per-claim, monthly, quarterly, and/or annual basis, depending on each individual patient’s health plan and other prescription drug costs.
Patient may not seek reimbursement from any other plan or program (Flexible Spending Account [FSA], Health Savings Account [HSA], Health Reimbursement Account [HRA], etc.) for any out-of-pocket costs covered by the Co-Pay Program. Patient or healthcare provider may be required to submit an Explanation of Benefits (EOB) following each infusion to the Co-Pay Program.
The Co-Pay Program only applies in the United States, including Puerto Rico and other U.S. territories, and does not apply where prohibited by law, taxed, or restricted. This does not constitute health insurance. Void where use is prohibited by your insurance provider or health plan. If your health plan changes you must notify EntyvioConnect at 1-844-368-9846. This offer is not transferable and is limited to one offer per person and may not be combined with any other coupon, discount, prescription savings card, rebate, free trial, patient assistance, co-pay maximizer, alternative funding program, co-pay accumulator, or other offer, including those from third parties and companies that help insurers or health plan manage costs. Not valid if reproduced.
By utilizing the Co-Pay Program, you hereby accept and agree to abide by these terms and conditions. Any individual or entity who enrolls or assists in the enrollment of a patient in the Co-Pay Program represents that the patient meets the eligibility criteria and other requirements described herein. You must meet the program eligibility requirements every time you use the program.
Insurance support
Now that your patients have been prescribed
ENTYVIO, EntyvioConnect offers your patients support
throughout the entire insurance approval process.
Contact us for support with:
- Benefits investigation
- Prior authorization (PA) assistance
- Appeals and denials assistance
Affordability
The support team at EntyvioConnect understands
that each patient’s financial circumstances are unique,
which is why we work closely with eligible patients to
help them afford their treatment.
- Co‑Pay Program: If eligible, patients who
have health insurance through their
employer or purchased a plan on their own
can pay as little as $0 per dose, up to the
maximum annual program benefit. Terms
and conditions apply†- Available for both IV infusions and SC
injections
- Available for both IV infusions and SC
- For patients with Medicare, Medicaid, or
TRICARE (government-funded health insurance):
the Co-Pay Program is not available. For these
patients, the support team at EntyvioConnect
will review benefits and potential financial
options outside of the Co-Pay Program - Patient Assistance Program: Patients with
no health insurance or for those whose
benefits are insufficient to cover ENTYVIO
may receive treatment at no cost if they
meet certain eligibility requirements
Financial Assistance
Reimbursement
The EntyvioConnect Co-Pay Program ("Co-Pay Program") provides financial support for commercially insured patients who qualify for the Co-Pay Program. Participation in the Co-Pay Program and provision of financial support is subject to all Co-Pay Program terms and conditions, including but not limited to eligibility requirements, the maximum benefit per claim and the Maximum Annual Benefit. By enrolling in the Co-Pay Program, you agree that the program is intended solely for the benefit of you—not health plans and/or their partners. Further, you agree to comply with all applicable requirements of your health plan. The Co-Pay Program cannot be used if the patient is a beneficiary of, or any part of the prescription is covered by: 1) any federal, state, or government-funded healthcare program (Medicare, Medicare Advantage, Medicaid, TRICARE, etc.), including a state pharmaceutical assistance program (the Federal Employees Health Benefit (FEHB) Program is not a government-funded healthcare program for the purpose of this offer), 2) the Medicare Prescription Drug Program (Part D), or if the patient is currently in the coverage gap, or 3) insurance that is paying the entire cost of the prescription. Takeda reserves the right to change or end the Co-Pay Program at any time without notice, and other terms and conditions may apply.
If you have enrolled in an accumulator adjustment, co-pay maximizer, or similar program that purports to help manage costs or later learn that your insurance company or health plan has implemented such a program, you agree to inform EntyvioConnect at 1-844-368-9846. In an accumulator adjustment program, payments made by you that are subsidized by a manufacturer co-pay assistance program do not count toward your deductibles and other out-of-pocket cost-sharing obligations. In a co-pay maximizer program, the amount of your out-of-pocket cost obligation is increased to match support offered by a manufacturer co-pay assistance program. It may be possible that you are unaware whether you are subject to these programs when you enroll in the Co-Pay Program. Takeda will monitor program utilization data and reserves the right to discontinue assistance under the Co-Pay Program at any time if Takeda determines that you are subject to a co-pay maximizer, accumulator, or similar program.
The Maximum Annual Benefit under the Co-Pay Program is subject to change without notice. Subject to all terms and conditions, the Maximum Annual Benefit under the Co-Pay Program may be applied to out-of-pocket cost for your ENTYVIO prescription, including co-pay, co-insurance or deductible. The Co-Pay Program is for medication costs only and does not include costs to give you your treatment. Subject to all terms and conditions, the Maximum Annual Benefit under the Co-Pay Program is $20,000 per calendar year. However, except where prohibited by law, if your insurance company or health plan implements a co-pay maximizer program or similar program, you will have a reduced Maximum Annual Benefit of $9,000 per calendar year. If your insurance company or health plan removes ENTYVIO from such program, subject to all terms and conditions, you will be eligible for co-pay assistance up to the Maximum Annual Benefit for patients who are not subject to maximizer adjustment or similar programs.
The actual application and use of the benefit available under the co-pay assistance program may vary on a per-claim, monthly, quarterly, and/or annual basis, depending on each individual patient’s health plan and other prescription drug costs.
Patient may not seek reimbursement from any other plan or program (Flexible Spending Account [FSA], Health Savings Account [HSA], Health Reimbursement Account [HRA], etc.) for any out-of-pocket costs covered by the Co-Pay Program. Patient or healthcare provider may be required to submit an Explanation of Benefits (EOB) following each infusion to the Co-Pay Program.
The Co-Pay Program only applies in the United States, including Puerto Rico and other U.S. territories, and does not apply where prohibited by law, taxed, or restricted. This does not constitute health insurance. Void where use is prohibited by your insurance provider or health plan. If your health plan changes you must notify EntyvioConnect at 1-844-368-9846. This offer is not transferable and is limited to one offer per person and may not be combined with any other coupon, discount, prescription savings card, rebate, free trial, patient assistance, co-pay maximizer, alternative funding program, co-pay accumulator, or other offer, including those from third parties and companies that help insurers or health plan manage costs. Not valid if reproduced.
By utilizing the Co-Pay Program, you hereby accept and agree to abide by these terms and conditions. Any individual or entity who enrolls or assists in the enrollment of a patient in the Co-Pay Program represents that the patient meets the eligibility criteria and other requirements described herein. You must meet the program eligibility requirements every time you use the program.
THE START PROGRAM
No cost.
Zero enrollment delays.
For up to 3 years.
After prescribing ENTYVIO, the Start Program is a fast and easy way to ensure your eligible commercially insured patients get access to ENTYVIO IV or the ENTYVIO Pen when there are delays in the insurance process.
For ENTYVIO patients whose prior authorization was denied by their health plan: The Start Program offers ENTYVIO for both IV infusions and the ENTYVIO Pen at no cost for up to 3 years while the appeals process is pending.
Eligibility requirements apply.
Terms and conditions apply.
IV=intravenous.
The ENTYVIO Pen is an option
after at least 2 IV infusions.
Bridge Program
For patients with a temporary gap in commercial coverage or authorization (job loss, insurance transition):
Bridge Program offers ENTYVIO at no cost for up to 6 months. Available for IV Infusions or SC Injections
Eligibility*:
- Patient must have been on ENTYVIO prior to coverage loss
- ENTYVIO coverage was from a commercial health plan
- Available for IV infusions or the ENTYVIO Pen
Terms and conditions apply.
*Additional eligibility requirements apply.
Hear an office manager’s experience with the Bridge Program
Words that come to mind when I think about insurance: frustrating, time consuming, and inconvenient for my patients.
My main challenge that my patients face would be insurance not approving the medication.
The Bridge Program has been an extreme help for my patients.
Especially with COVID hitting and happening. Patients lost insurance, changed jobs, and the Bridge Program was able to step in and allow them to continue their medication without interrupting treatment.
It’s easy to use. There is a resource online that allows them to review the application. We also work really close with the patients to get the signatures, basically, to provide this medication for up to 6 months.
I work with EntyvioConnect because I like to ask questions to find the right programs fit for my patients.
Do you have an EntyvioConnect experience to share?
Patient education
Nurse Educators
Patients can opt in to be paired with a Nurse
Educator and receive guidance and resources
throughout their treatment on ENTYVIO. Nurse
Educators support patients by:
- Following up at regular intervals during
treatment - Providing general information on ENTYVIO and
practical tips for living with their condition
- Helping to identify treatment, health, and lifestyle
goals to discuss with their doctor - Providing injection education in-home or virtually
via an online secure platform
Nurse Educators do not provide medical advice.
Injection Education Kit
- ENTYVIO SC formulation is intended for self-administration or administration by a caregiver. The patient or caregiver should be trained by a healthcare professional
- Patients can request an injection education kit
that includes a training guide, demo pen, alcohol
wipes, and more. These materials come with a
portable cooler they can use to take their
medication with them wherever they are. An
accompanying support site dedicated to ENTYVIO
pen users offers training videos plus an option to
sign up for text reminders - Speak to a Patient Support Manager to request a kit for your patient
EntyvioConnect offers a range of programs tailored
to help patients with access and affordability once
the prescribing decision is made.
Billing and coding for ENTYVIO
One of the most common reasons for prior authorization denial is the inclusion of an incorrect billing code. It is important to be accurate with coding for the product, administration, and associated procedures. Here are the most common codes to use when submitting documentation to your patient’s health plan.
The following coding information is intended as general information only. Please refer to your patient's payer's policies for specific billing guidance.
| ENTYVIO | 64764-300-20* | 300 mg single-dose vial in individual carton |
| ENTYVIO | 64764-108-21 | 108 mg single-dose prefilled pen in individual carton |
*Proper billing may require code conversion to 11-digit format: 64764-0300-20.
| J3380 | ENTYVIO |
| J3380 | Injection, vedolizumab, intravenous, 1 mg |
| 96365 | IV Infusion, up to 1 hour |
| 96413† | Chemotherapy, IV Infusion, up to 1 hour |
| 96372 | Therapeutic, prophylactic, or diagnostic injection; subcutaneous injection or intramuscular |
†Certain Medicare contractors do not allow the use of procedure code 96413 (Chemotherapy, intravenous (IV) Infusion, up to 1 hour) for administration of ENTYVIO. As applicable, healthcare provider should consult the Medicare contractor to determine which code is most appropriate, or call EntyvioConnect for assistance at 1-855-ENTYVIO.
Ulcerative colitis
| K51.00 | Ulcerative (chronic) pancolitis without complications |
| K51.20 | Ulcerative (chronic) proctitis without complications |
| K51.30 | Ulcerative (chronic) rectosigmoiditis without complications |
| K51.50 | Left sided colitis without complications |
| K51.80 | Other ulcerative colitis without complications |
| K51.90 | Ulcerative colitis, unspecified, without complications |
Crohn’s disease
| K50.00 | Crohn’s disease of small intestine without complications |
| K50.10 | Crohn’s disease of large intestine without complications |
| K50.80 | Crohn’s disease of both small and large intestine without complications |
| K50.90 | Crohn’s disease, unspecified, without complications |
ICD-10-CM=International Classification of Diseases, Tenth Revision, Clinical Modification
Explore more topics
Hear expert perspectives on ENTYVIO
Need to refer a patient to an infusion center?
The content on this page has been written and
reviewed by Takeda.
References:
- ENTYVIO (vedolizumab) prescribing information. Takeda Pharmaceuticals.
- HCPCS.codes. Accessed February 15, 2023. https://hcpcs.codes/j-codes/J3380/
- CMS.gov. Accessed February 15, 2023. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/
PFS-Federal-Regulation-Notices-Items/CMS-1715-5 - CMS.gov. Accessed February 15, 2023. https://www.cms.gov/medicare/icd-10/2021-icd-10-cm